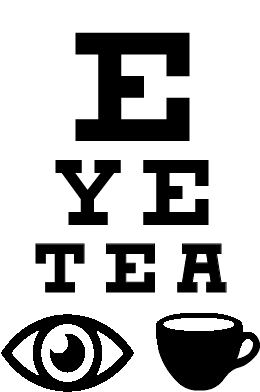
Ophthalmology’s battle with scope creep: what a new physician should know
Authors: Bhakti Panchal, BS and Whitney Stuard, MD, PhD
The world of ophthalmology has always been intertwined with the world of optometry. While ophthalmologists may work closely with optometrists in clinical settings, there are distinct differences between their skill sets. Both ophthalmologists and optometrists receive years of schooling to be licensed to provide different types of eye care (Table below). 1 Optometrists commonly perform tasks such as prescribing glasses or contact lenses and providing some forms of routine vision care. Most ophthalmologists, also known as eye physicians and surgeons, receive surgical training in addition to their comprehensive medical treatment of eye diseases.
-
Undergraduate Studies | Four years of college or university
Graduate School | Four years of medical school - allopathic (M.D.) or osteopathic (D.O.)
Post Graduate Training | Four years of residency followed by one to two years of fellowship training
-
Undergraduate Studies | Four years of college or university
Graduate School | Four years of optometry school
Postgraduate Training | One year of residency
While the training of ophthalmologists and optometrists is different over the past decade there has been an increasing level of disagreement about each group's scope of practice. The rise of non-physicians, such as optometrists, being allowed to provide physician-level care is a concerning trend called “scope creep”. Scope creep in health care is essentially non-medically trained practitioners, who have not met the qualifications and training for unrestricted licensure to practice medicine, attempting to expand their level of patient care to include the care customarily given by residency-trained physicians.
Ophthalmology is not the only specialty affected by scope creep. Anesthesiology, family medicine, emergency medicine, and psychiatry are some of the specialties being attacked by unrelenting attempts to expand scope, by nurses and physician assistants. The American Medical Association (AMA) has led a coalition of over 100 national, state, and specialty societies to combat these dangerous bills across the United States.2 AMA Scope of Practice Partnership in particular works to educate lawmakers and the public about why scope creep is dangerous to patients.2
Scope Creep in Ophthalmology
Just as other fields in medicine are experiencing the increased involvement of physician assistants and nurse practitioners stepping in for traditional physician roles, ophthalmology has also been affected. For example, in ophthalmology, some states have allowed optometrists to perform procedures that only ophthalmologists are appropriately trained to perform. This includes glaucoma laser (trabeculoplasty or SLT) and YAG capsulotomy procedures. This is concerning and can be harmful to patient care.
Concerning scope creep, Dr. Kelly Green, MD, and board-certified ophthalmologist in Texas says “In reality, we are protecting patients from harm and the practice of medicine by non-physicians. In our field, this involves optometrists attempting to legislate themselves into a position of being able to ‘do medical’ eye care. As non-MDs, optometrists simply do not have the breadth and depth of understanding of the anatomy, physiology, and pathophysiology of the human eye.”
National Initiatives and State Legislation
Scope creep-based bills and legislative attempts are being submitted in various states each year to expand the scope of practice of non-physicians into a position to perform services and procedures previously deemed only safe to be performed by residency-trained physicians. Currently, each state delineates the scope of practice of optometrists, and this has become a serious concern for those in medicine and ophthalmology. A study published in JAMA Ophthalmology reported the outcomes of ophthalmologists and optometrists after performing laser trabeculoplasty (SLT) procedures in Oklahoma. According to the article, the laser procedure performed by an optometrist had twice the likelihood of having to re-perform the laser surgery in the corresponding eye compared to ophthalmologists. 3 Additionally, when compared to ophthalmologists, optometrists had an 189% increased risk of having patients undergo additional laser procedures in the same eye.3 The American Academy of Ophthalmology (AAO) is actively involved in this issue stating, “Statistics show that safety risks to patients are far too great to grant certain surgical authorities to health care practitioners who lack adequate training and expertise as a primary surgeon.”4 They currently operate the Surgical Scope Fund to help ensure patient safety through surgical standards.
After dozens of attempts in a variety of states over the years, Oklahoma, Kentucky, Louisiana, Alaska, Arkansas, Louisiana, and Indiana have been noted as states that allow optometrists to perform some sort of laser surgery.5 Each year new bills asking for these expansions are submitted in additional states or resubmitted in states where the efforts have previously failed, making it a continual battle.
With the help of the AMA and AAO’s Surgical Scope Fund, some states have successfully prevented these bills from being passed. The most recent and notable event was last year in 2022 when the state of California was presented with an optometry-sponsored bill that would allow optometrists to perform ocular surgeries. With the bill being passed by 1 vote in the state assembly, it was passed on to Gavin Newsom, the governor of California, who had the final say. By having the AMA and California State Society advocate for their patients, the bill was vetoed with Governor Newsom’s response stating, “I am not convinced that the education and training required is sufficient to prepare optometrists to perform the surgical procedures identified.”6
Do No Harm
While everyone in the health care team is important and has a role, it is also important that these physicians and non-physicians practice within their scope and provide safe care. Above all else physicians have each vowed, at the start of their years-long educational journey, to “do no harm.” More and more, physicians are waking up to the reality that they must ensure patient safety and fight for what is best for their patients, in the clinic or operating room, or even on the floor of the state house or senate.
When asked, “What can residents and students do to help prevent scope creep?”
“Join your state ophthalmology society. Sometimes membership is free for students or residents! Get to know YOUR state representative and senator.”
Dr. Green says: “Join your state ophthalmology society. Sometimes membership is free for students or residents! Get to know YOUR state representative and senator.” Furthermore, AAO holds its Mid-Year Forum and Congressional Advocacy Day in Washington D.C. every year. This meeting allows physicians, residents, and students from across the country to meet with legislators and continue to advocate on behalf of their patients. This is a great way for medical students and resident physicians or fellows to get involved with their state society and in the issues surrounding the scope of medical practice.
References
Differences in education between optometrists and ophthalmologists. Differences in Education Between Optometrists and Ophthalmologists - American Academy of Ophthalmology. (2011, May). https://www.aao.org/about/policies/differences-education-optometrists-ophthalmologists
American Medical Association, & Robeznieks, A. (2022, June 13). Inside the AMA’s wide-ranging fight against scope creep. American Medical Association. https://www.ama-assn.org/practice-management/scope-practice/inside-ama-s-wide-ranging-fight-against-scope-creep
Stein, J. D., Zhao, P. Y., Andrews, C., & Skuta, G. L. (2016). Comparison of Outcomes of Laser Trabeculoplasty Performed by Optometrists vs Ophthalmologists in Oklahoma. JAMA ophthalmology, 134(10), 1095–1101. https://doi.org/10.1001/jamaophthalmol.2016.2495
Surgical Scope Fund - American Academy of Ophthalmology. (n.d.). Surgical Scope Fund. https://www.aao.org/advocacy/surgical-scope-fund/overview
Jones, L., Konstantakopoulou, E., & Gazzard, G. (2021). Selective laser trabeculoplasty (SLT) performed by optometrists for patients with glaucoma and ocular hypertension: a scoping review. BMJ open ophthalmology, 6(1), e000611. https://doi.org/10.1136/bmjophth-2020-000611
Radical bill vetoed on safety grounds. American Medical Association. Optometrists doing eye surgery? Radical bill vetoed on safety grounds